What Is the Ludwig Scale?
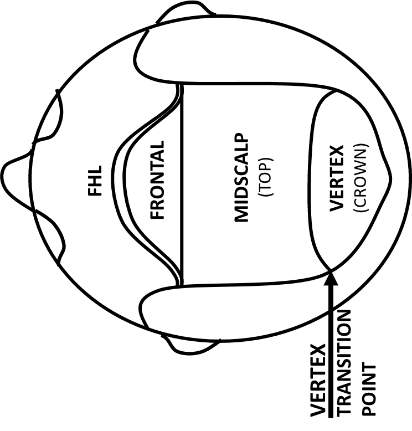
Female-pattern hair loss (FPHL), also called androgenetic alopecia, is the most common form of hair loss in women. The areas prone (frontal forelock, mid-forelock, and vertex) to thinning secondary to androgenetic alopecia are shown in the below graph.
FPHL is an aging process that affects every female with progressive thinning as they age. A patient’s genetics will dictate the severity of hair loss. By the age of 50 years old, approximately 25% of women have a decrease in hair density below 50%, where it becomes noticeably see-through to the human eye. Women notice their hair loss way before it’s noticeable to the human eye because they notice the volume in their ponytail is thinner and thinner as they age. This is a telltale sign of the progressive nature of FPHL. This hair loss can have significant psychosocial effects since the individual may be perceived as less attractive and older.
The progressive miniaturization of the hair shaft is identical in both men and women experiencing androgenetic alopecia; however, the clinical pattern of hair loss differs significantly between men and women. Unlike men, most women experiencing FPHL still retain the frontal hairline (FHL) and do not follow the Norwood stages typically seen in male pattern hair loss. Therefore, it became necessary to develop a classification system to determine the extent of FPHL to more accurately treat and assess the progression. In 1977, Dermatologist Dr. Ludwig classified FPHL into 3 grades of progressively worsening hair loss.
Also Read: Norwood Hair Loss Scale: Stages & Treatment Options
Importance of the Ludwig Scale
The Ludwig classification system is essential in order to develop medical studies evaluating the medical and surgical treatments for female pattern hair loss. It is also essential in developing the medical and surgical plan for each individual patient. I tell my patients experiencing significant female pattern hair loss that the treatment is not “one and done”, but the treatments need to be continued to maintain the effects in this journey of aging, which is intimately intertwined with the progressive hair thinning. As a physician, it is imperative to understand that the younger a patient starts thinning, the more likely they will end up with the most advanced grade on the Ludwig scale. This is why it is of the utmost importance for the physician to convey the need for the preventative medical treatments (minoxidil, off-label antiandrogens & androgen modulators) in slowing the progressive nature of female pattern hair loss. This foresight is also fundamental in deciding if hair transplants will be able to accomplish the patient’s goal acutely and/or long-term. It is incumbent on every physician treating hair loss to make a diagnosis, to educate the patient on the pros and cons of the various treatment modalities and their limitations, and, lastly, to make sure they are realistic about their expectations.
The 3 Stages of the Ludwig Scale
The stages of the Ludwig scale are outlined below. Each will be examined in detail to highlight its characteristics and treatment options.
Grade I

Identification
Grade I is the beginning phase of perceptible thinning behind the frontal hairline, 1-3 cm, and extending back to the vertex. In this grade, female patients notice increased widening of their hair part-line and a decreased volume in their ponytail.
Treatment Options
It is imperative to make the diagnosis of FPHL early and initiate the preventative medical therapies (i.e., minoxidil, antiandrogens, androgen modulators) as soon as possible. I tell my patients not to judge results on a stopwatch but rather on a calendar year. It often takes 1-2 years to see a therapeutic response. I also tell patients that therapeutic results should not be judged on what you see but rather what you do not see (i.e., further balding). Patients need to be counseled that the treatment needs to be continued to slow the progressive nature of FPHL. If a patient stops the medical therapies, she will lose the results. Hair transplants to increase the density can be quite beneficial in meeting a patient’s goal.
Grade II
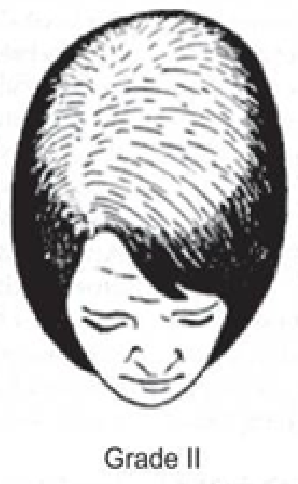
Identification
Grade II is a pronounced thinning across the top of the head with an obvious widening of the part line within the hair.
Treatment Options
In this stage of hair loss, the preventative medical therapies are still very important in slowing the progression of hair loss. However, hair transplants may be necessary to bring back the desired density. It is very important that the patient understands the hair transplant’s limitations of supply & demand. There is a limited and fixed amount of thick, good genetic hair we can take from the sides and back of the scalp to transfer to the balding region. The more extensive the balding, the more likely it is that there will not be enough good genetic hair to cover everywhere; therefore, it is important for patients to be realistic about their goals and place this limited good genetic hair in the most cosmetically important areas (the frontal forelock).
Grade III
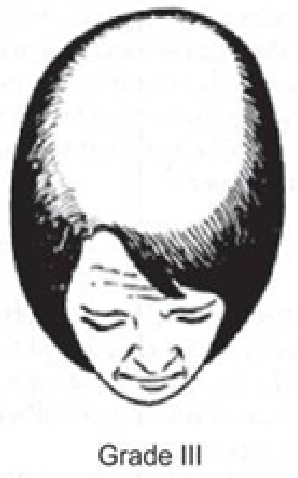
Identification
Grade III is the most advanced grade of the Ludwig scale. There is almost complete loss of hair (the miniaturized hairs become imperceptible to the human eye). The frontal hairline is still intact.
Treatment Options
At this end stage, Ludwig grade, the medical and surgical treatments have a very limited role since most patients’ goals will not be attained. At this late Ludwig stage, many patients elect to treat their hair loss with camouflaging agents or hair pieces.
Limitations of the Ludwig Scale
Over the decades, there have been many studies to try to create the ideal classification system for androgenetic alopecia in females; however, there are vastly different genetics in the human population. Therefore, there is no perfect classification that encompasses all female hair loss patterns. The Ludwig Classification is the most widely used for women with androgenetic alopecia. The other problem with the Ludwig grades is that it’s not exactly quantifiable where one grade starts and another grade ends. Furthermore, the Ludwig grades do not take into account women who have diffuse androgenetic alopecia, which involves miniaturization even on the sides and back of the scalp. When it comes to androgenetic alopecia, there is one constant: no matter what the pattern an individual follows, the hair loss progressively worsens as one ages.
My Experience
I am a clinical professor in the department of dermatology at USC School of Medicine, teaching the medical residents the latest advances in the medical and surgical treatments of all the different forms of hair loss. Hair loss is a symptom and not a diagnosis, similar to stomach pain. There are many different causes of hair loss. Therefore, it is of the utmost importance for a female experiencing hair loss to be diagnosed correctly by a dermatologist. This diagnosis will shed light on what is the cause of hair loss and will also dictate the treatment course.
After making the diagnosis of FPHL (androgenetic alopecia) and determining their Ludwig grade, it is important for patients to understand that there is no perfect cure. The patient should be thoroughly counseled and educated on the cause and their treatment options: 1) cosmetic treatments (i.e., camouflage, hair extensions, hair pieces), 2) medical treatments (i.e., minoxidil, antiandrogens, androgen modulators), and 3) surgical treatments (i.e., hair transplants). After gaining this knowledge, the patient can make an informed decision on attaining her treatment goals.
Hair transplants have greatly increased in popularity in women experiencing the different Ludwig grades. When properly informed, patients develop realistic goals and are very happy with their hair transplant results.
Worried About Hair Loss? Let’s Talk.
Get trusted answers from Dr. McAndrews, a board-certified hair restoration physician with over 20 years of experience. We offer both FUE and FUT hair transplants in Los Angeles at our Pasadena office and offer convenient online consultations that you can reserve from anywhere.
Sources
- Ludwig E. Classification of the types of androgenetic alopecia (common baldness) occurring in the female sex. Br J Dermatol. 1977;97:247–54. doi: 10.1111/j.1365-2133.1977.tb15179.x. [DOI] [PubMed] [Google Scholar]
Dr. Paul J. McAndrews is a world-renowned expert in hair loss and hair restoration, and one of only two physicians to have served as President of both the ISHRS and the ABHRS. He is a Clinical Professor at USC/LAC Medical Center and an Expert Medical Reviewer for the California Medical Board, with more than 20 years of experience performing hair transplant procedures, including both FUE and FUT. Serving patients throughout Los Angeles and Southern California, he is regarded as one of the best hair transplant specialists in Los Angeles.
